Post-Craniectomy PICU Stay
Lots of moms who have babies going through this surgery say
the wait while the baby is in the OR is the worst part. It wasn’t that way for
me. It sucked, but honestly, I just laid down on a bench and tried to sleep. A
few hours later Dr. Smartt came out and told us they were done and everything
looked great. He did have to receive a blood transfusion (not always necessary
with the short endoscopic surgery) as his hemoglobin was low to begin with,
probably due to his frequent blood draws, but other than that everything went
100% normally. Someone directed us up to the PICU floor and we FINALLY got to
go in and see him. The first thing I noticed was he was sniffling like you do
after you’ve been crying hard for a long time and you can’t catch your breath.
I felt so guilty we couldn’t be there earlier to comfort him. His head looked
pretty brutal, with WAY more of his head shaved than I expected and dried
iodine and blood (mostly iodine) all over the two zigzagged scars that now
decorated his head. He was pretty out of it, he would wake up every few minutes
and let out a cry, but he just couldn’t stay awake for good. He was also on oxygen,
given to him through a nose cannula, because he wasn’t breathing strongly on
his own in the recovery room. The nurses gave us a bag of his hair since this
was technically his “first haircut.” I hadn’t even thought to ask about it, so
I’m very grateful they did that for us. If you’re going through this surgery
soon, ask for your baby’s hair!
 |
| His head shape was already noticeably different, about 40% of the total change comes from surgery alone |
 |
| If I weren't fundamentally opposed to ascribing traditional gender roles to babies, I would probably caption this "chicks dig scars." |
When he started to wake up, they gave him morphine
intravenously, and the trouble began. I’m the furthest thing from a medical
professional, so usually the computer screens with all the measurements on it
are lost on me. The only one I know about is oxygen saturation (I remember
watching my grandfather’s oxygen saturation levels when he was in the Mayo
Clinic years ago). All I know is, the closer the number is to 100, the better.
A few minutes after the morphine, Eli’s oxygen saturation levels began to drop
very quickly. There are always beeps and alarms going off on machines, but this
alarm was different. It was loud and very urgent sounding. I was sitting on a tall
rolling chair next to his bed talking to him and holding his hand, the next
thing I knew several nurses ran in and rolled me out of the way and started
giving him oxygen through a breathing mask. Will had run home to catch up on
some work, so it was me, my mom, my grandmother, and Will’s dad in the room. Apparently
I looked calm (Will’s dad made it a point to mention that to Will
later…probably because he saw me have a full blown panic attack when Will’s mom
was in the hospital towards the end of her life), but I was honestly just
staring at Eli, thinking I was about to watch him die right in front of me, and
how Will wouldn’t even be there when it happened. I remember my grandmother
coming over to try to hug me but I told her to stay away. I’m usually able to
keep my stoic face on, but once someone tries to comfort me or asks me if I’m
alright, I lose it. I can’t tell you how many times I have replayed this scene
over and over in my mind, or how many times it’s kept me up at night. It still
haunts me. I’ve never been the most maternal, nurturing person, but some nights
after Eli is asleep I go in his room and just watch him…and I don’t think I
would do so if it wasn’t for this harrowing ten minute experience. I can’t
accurately put into words what it felt like to be standing there thinking about
how much I would miss this little person I barely even got to know.
 |
| EKG leads |
A doctor called for an EKG, an X-ray, and had them draw
blood for a blood gas test. This took a few minutes, and in that time his
oxygen dropped a couple more times, but we were all prepared now and the nurses
acted very quickly in getting him oxygen. Finally the blood gas results came
back, and they explained to me that his CO2 was very high, and they wanted to
give him Narcan. I knew what Narcan was because of Will’s previous work as a
paramedic. It’s often given to addicts who have overdosed to wake them up. In very
simple terms, it removes the narcotic from the body. So it would remove the
morphine from his system. However, the doctor also said it would remove his
natural pain receptors as well. So it would be “excruciating” for Eli. That
wasn’t what I wanted to hear, but we really didn’t have a choice. They gave him
the Narcan and he started screaming almost immediately. To help with the pain
somewhat they also gave him some IV Tylenol, and this was all he was able to
have for the entirety of his recovery (both in the hospital, then Tylenol via
mouth at home).
At this point it was early evening and we still hadn’t been
able to hold him or feed him. I believe a nurse finally tried to feed him
around 8 PM that night (so about 24 hours after his last meal). Luckily the
rooms in the PICU are much better than the NICU, so Will and I eventually went
to sleep on the pull out couch next to Eli’s bed. The next day was mostly
uneventful. Lots of endoscopic surgery babies get to go home the day after
their surgery, but not us! We were FINALLY allowed to hold him around 4 PM on
Tuesday. Going that long (from early Monday morning to Tuesday afternoon) only
being able to hold his hand, still with gloves and gowns on like our NICU stay,
was terrible. The video below is Tuesday night. No food for an entire day, no morphine, a terrible experience the previous afternoon, and he still wanted to smile at me. We may have been unlucky with his health problems, but we have been SO lucky with his personality. He is truly such a happy baby and such a joy to be around.
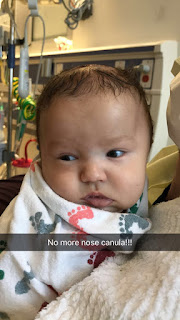 |
| Wednesday afternoon before we were discharged |
If anyone is reading this and going through the surgery: ask
your nurses what all you can take when you leave! Our nurse was amazing and let
us take EVERYTHING. All the formula that was made for him (the crazy expensive
specialty formula), the pacifiers they gave us (he actually uses those all the
time now, they are called Jollypops and hospitals use them because they allow
room for a nose cannula, unlike the ever popular Soothie pacifiers), extra
doses of Tylenol and calcium, the blankets and teddy bear he was given
post-surgery, his hospital gown (hopefully we won’t be needing that ever again,
but it’s an interesting souvenir), and my favorite, the baby bumper from his hospital
bed. It’s a long piece of heavy flexible material covered in foam and cloth,
and can be bent into different shapes to keep your baby from rolling around too
much. We kept it in a U-shape and had it around the bottom of Eli’s body so he
would remain on his back. I loved it and wanted to buy one, but when I googled
it I found they were $200! So my mom asked the nurse about it and she just gave
it to us. It was awesome. We used it for weeks afterward and I’m definitely
keeping it just in case we decide to have another baby.
Next up: the dreaded helmet.



Comments
Post a Comment